GYNAECOMASTIA: WHAT IS IT?
WHAT IS GYNAECOMASTIA?
Gynaecomastia is a common benign condition resulting in enlargement of male breast tissue. From a surgical point of view, it is best to define gynaecomastia as a persistent enlargement of male breast tissue. It is this permanent enlargement that motivates patients to seek surgical correction of the condition. Surgery offers an effective means of treating gynaecomastia. The best results are attained in patients with good skin tone and smaller breast enlargements, and weight stabilisation and diet are essential in preparing for surgery. The surgery seeks to treat the breast tissue primarily, with the hope that the skin envelope will retract to an aesthetically normal position following surgery.
Gynaecomastia is estimated to affect almost half of the male population at some time or another during life. Although organic causes, including normal physiological development during adolescence, hormonal imbalance, some medications and other medical conditions may be implicated, the vast majority of cases are labelled ‘idiopathic’, meaning that a cause cannot be found. Affected breast tissues, as well as the nipple–areola complex, become prominent and this may cause embarrassment and self-consciousness.
ASSESSMENT
HISTORY
The age of onset, time span of breast growth, pain and any regression or involution should be noted in the patient’s history. Alteration in patient weight and its effect on breast growth should also be documented. An enquiry should be made of any systematic symptoms such as weight loss, night sweats and anorexia. In particular, changes in olfaction or vision should be enquired about as this may suggest a pituitary tumour. Specific questions about medications should include drugs that cause gynaecomastia, including therapeutic and recreational.
CLINICAL EXAMINATION
Inspection from the front and side allow the surgeon to appreciate the extent of the disease globally, asymmetry of the breasts and to note any areolar widening and herniation. A testicular examination completes the assessment to exclude possible hormonally active tumours.
INVESTIGATIONS
It is rarely inappropriate to refer a patient with gynaecomastia to an endocrinologist for further investigation. Although pathologic gynaecomastia is uncommonly seen, ruling out underlying pathology is paramount to patient care. Investigations should be guided by the examination findings. General investigations may include evaluation of liver, renal and thyroid function (blood tests), as failure of these organs may cause gynaecomastia. Imaging can include a chest radiograph to exclude carcinoma of the lung, mammography of the breast to rule out breast cancer and CT head to exclude pituitary tumours.
MANAGEMENT
When a recent diagnosis of idiopathic gynaecomastia has been made, it is reasonable to delay definitive surgical management, as spontaneous regression is likely. This is particularly so in adolescent gynaecomastia.
It is also prudent to delay surgical management in those with a body mass index greater than 28kg/m2. Obesity will not only exaggerate the degree of breast enlargement and lead to increased ptosis, but also increase perioperative risk with regards to infection, wound breakdown and thromboembolic events.
NON-OPERATIVE TREATMENT
Once a pathological cause of gynaecomastia has been excluded (either clinically or through further investigations) a watch and wait policy is always prudent as some cases may resolve.
Possible non-operative treatments:
- Anti-oestrogen tamoxifen has been reported to be effective in some cases of gynaecomastia
- Clomiphene (however the results of clomiphene treatments are disappointing)
- Danazol has proved effective in management of gynaecomastia (however there can be adverse effects such as weight gain)
OPERATIVE TREATMENT WITH DR FARHADIEH
BEFORE YOUR GYNAECOMASTIA PROCEDURE:
During your initial consultation Dr Farhadieh will note a detailed medical, drug and family history, including investigations you may have had in search of a cause. Your chief areas of concern, along with your expectations from surgery, will be discussed. The surgical procedure can be undertaken as a day procedure under general anaesthetic or sedation depending on the case, your preference and your surgeon’s recommendation. The actual operation generally takes between 1 and 2 hours.
Surgery usually involves liposuction of the excess breast tissue, and most often entails a small resection of the breast tissue through an incision near the nipple–areola complex. In extreme cases the entire breast tissue may need to be surgically resected, including part of the skin envelope. Most surgeons, including Dr Farhadieh, prefer to take a conservative approach, resecting less rather than more tissues, and, if need be, performing smaller revisions later on.
For smokers, cessation of smoking 3–6 weeks prior to surgery and abstention for at least 3–6 weeks after the operation is recommended. Medications and herbal supplements that may increase the risk of bleeding should be stopped at least 2 weeks prior to surgery; they may be recommenced 1 week after surgery.
AFTER YOUR GYNAECOMASTIA PROCEDURE:
After your surgery, you will be taken to the recovery area and your chest will be dressed tightly. The dressings remain intact until you see your surgeon during a follow-up consultation in 10–14 days. Application of local anaesthetic will reduce immediate postoperative discomfort and small amounts of pain relief medication will be prescribed on discharge. These are often only necessary during the first few days postoperatively. Depending on your occupation you may be off work for 1–2 weeks. Your chest will be bruised for at least 1–2 weeks.
As with all surgery, there are potential complications, but fortunately these are not common. Dr Farhadieh will discuss these with you in detail during your consultation.
Your relationship with your surgeon is the most important part of the process. At any stage prior to or after your operation Dr Farhadieh and his staff will be available for advice and support. We are dedicated to being there for every step of your journey.
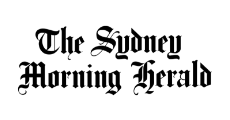
Gallery

30 year old male at 3 months post operatively who gynaecomastia treated with liposuction.
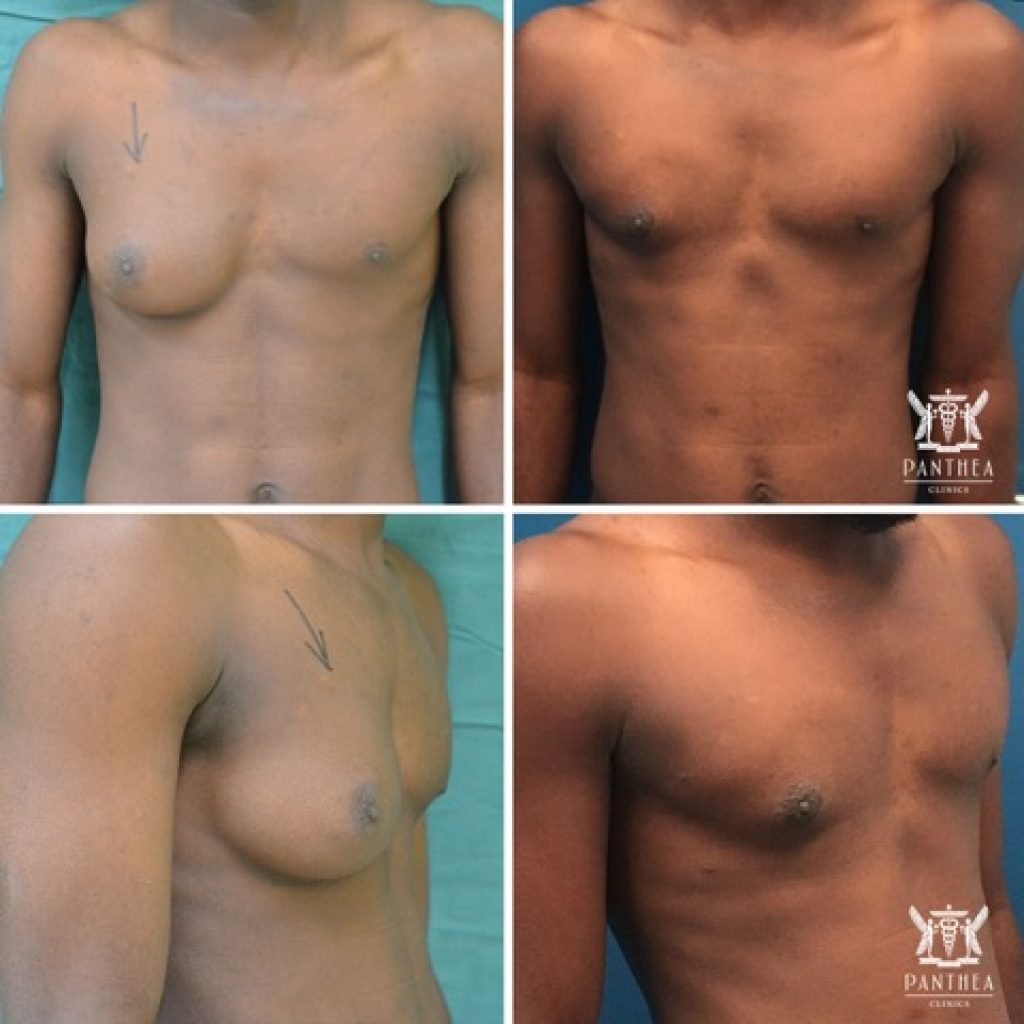
Unilateral gynaecomastia treated with liposuction and subcutaneous mastectomy in a 22 year old man at 12 months postoperatively.
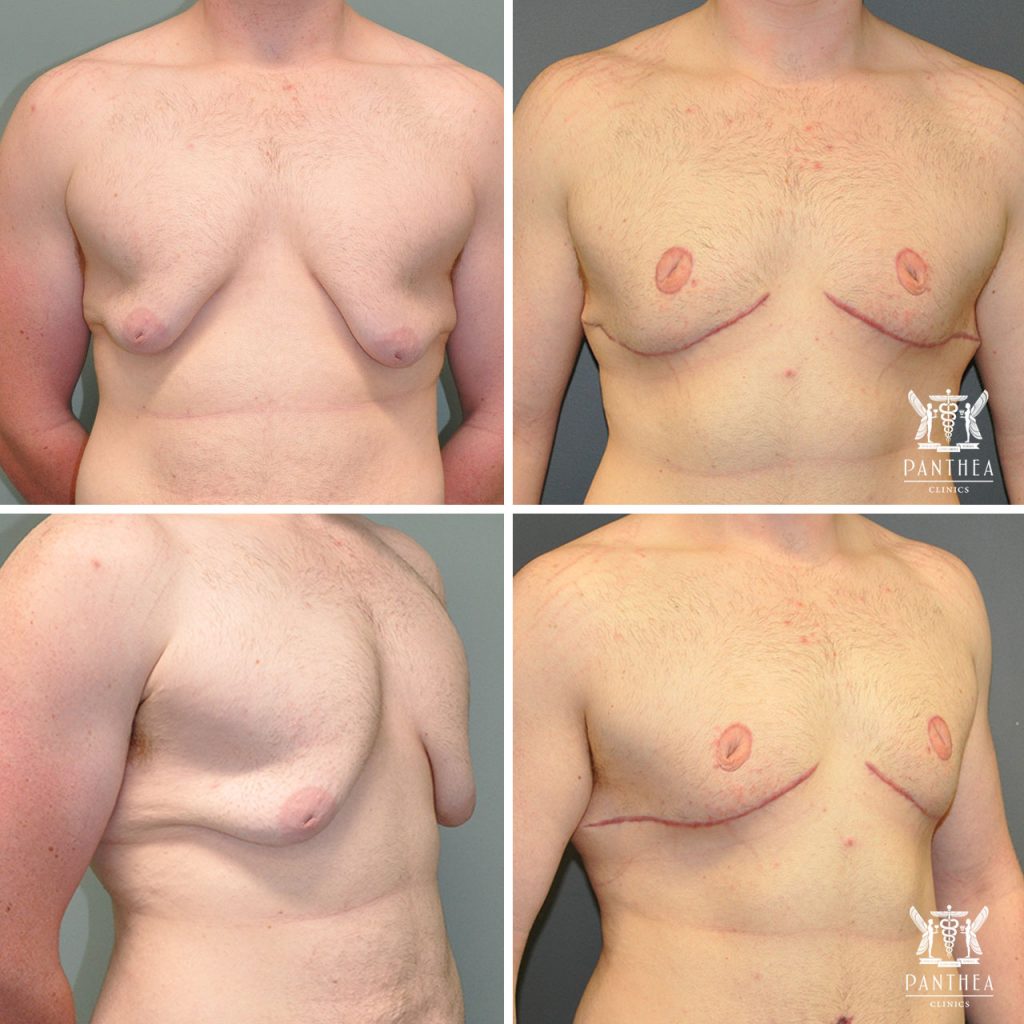
20 year old male at 3 months post operatively who gynaecomastia.

Bilateral gynaecomastia treated with liposuction at 3 months postoperatively.