BREAST RECONSTRUCTIONS: DECONSTRUCTED
WHAT IS BREAST CANCER?
Breast cancer is now considered to be the most common invasive cancer, and is clearly a global phenomenon of almost epidemic proportions. In terms of incidence, it is predicted that 1 in 8 Australian women will be diagnosed with breast cancer. Rates have steadily increased by around 1 to 2 % per annum from the 1980’s, although that has been explained by the widespread use of the mammography screening. The impact on health care systems remains immense for treatment as well as restoration.
RISK FACTORS:

TREATMENT
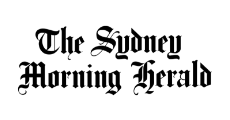
Surgical treatment followed by radiation and/or chemotherapy remain the main stay of treatment. The surgery often involves lumpectomy where the cancer is removed and the breast is then treated with radiation. Where mastectomy is needed (total) removal of the breast tissue then reconstruction options become essential.
Cancers can travel to local lymph nodes and spread so often a sentinel node biopsy is performed to sample and see if the node is positive, in these cases the remainder lymphatic basin is removed and postoperative radiotherapy is most often needed.
CHEMOTHERAPY
The surgical and medical treatment of breast cancer is individualized. Factors that are taken into consideration in the administration of adjuvant chemotherapy are the size of the invasive component of the primary tumour, the nodal status, hormone receptor expression, and human epidermal growth factor receptor 2 (HER-2/neu) expression. Histologic parameters that are taken into consideration as well are the lymphovascular invasion and histologic grading.
Adjuvant chemotherapy is administered for 3 to 6 months and it includes a combination of different medication. It has been successful in demonstrating reduction in recurrence rates and improvement of the survival outcome. An overview of the randomized trials on administration of adjuvant chemotherapy, in early- stage breast cancer, showed a substantial reduction of 5-year recurrence rate and 15-year mortality rate regardless of the estrogen receptor status of the primary cancer.
The implications of chemotherapy on reconstruction have been comprehensively reviewed in a meta-analysis by the American Society of Plastic Surgeons. There is no consistent finding that preoperative chemotherapy is a significant risk factor for complications in expander/implant reconstructions. It is advised that adjuvant chemotherapy should be completed 4-6 weeks prior to reconstructive surgery, and that adequate white cell level should be confirmed preoperatively. There is no definite data on effects of chemotherapy on autologous reconstruction.
PROGNOSIS
Prognostic factors include the status of axillary lymph nodes (number of nodes involved), tumour size, lymphatic or vascular invasion, age, histological grade, histological subtype, and response to adjuvant treatment.
The key objective in breast cancer treatment remains that of complete local cancer tissue removal such as to prevent recurrence or wider spread, and to treat more widespread disease. Complete surgical excision with negative margins remains the principle method of treatment and can be curative in patients with early disease, with adjuvant therapy (chemotherapy and radiotherapy) used to treat micrometastases.
ONCOLOGICAL-SURGICAL TREATMENT
MASTECTOMY
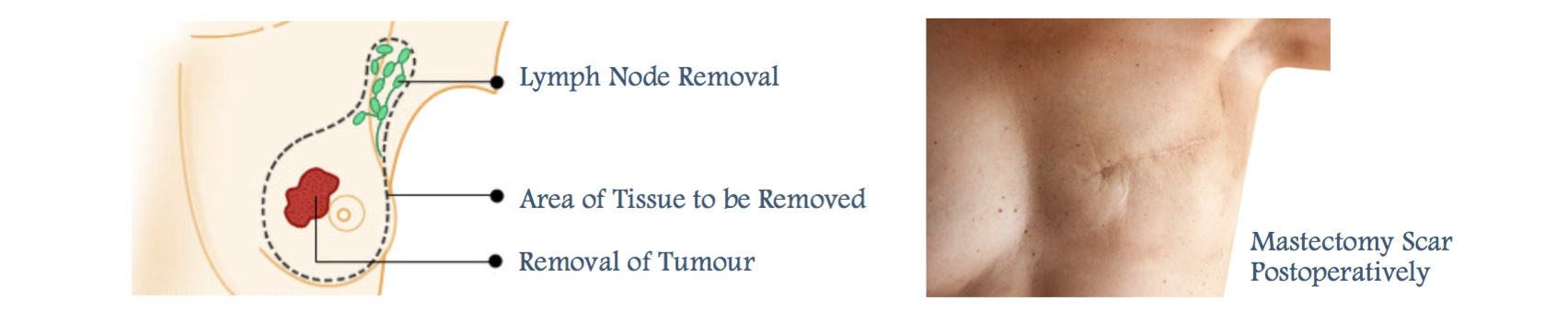
Breast cancer surgery has its origins in a necessarily aggressive technique developed by Halsted in 1882, without reconstruction in mind, and with extensive tissue clearance and impressive chest wall scarring. This en bloc removal of all breast tissue and pectoralis major muscle including the axillary nodes (and/or internal mammary lymph nodes), was modified by Patey to a procedure where the pectoralis major muscle was spared and then further to a “simple” or “total” mastectomy where all breast tissue including the skin and Nipple Areolar Complex (NAC) was removed, possibly accompanied by the ipsilateral axillary lymphatics.
In modern times, the appreciation of the wider and complex ramifications of breast cancer treatment has brought with it the now universal acceptance that the disease should be managed by an oncological team. The disfiguring consequences of the surgery, and the development of surgical techniques to reduce this, has prompted cancer surgery to evolve to facilitate reconstruction. Increasingly, the standard preservation of the IMF and superolateral fold, a useful residue of skin envelope, has been supplemented with preservation of even the areola or NAC (SSM or skin sparing mastectomy) which confers a greater likelihood of achieving symmetry.
Importantly, reviews have shown that a skin-sparing periareolar subcutaneous mastectomy does not increase the likelihood of local recurrence. The advantages of the SSM are the judicious use of native skin with its preferential colour and texture match, the retention of the breast foot-print, and critical elements of the skin envelope. There may be less need for surgery to the contralateral breast, and a smaller reconstructive skin paddle may be required. Surgical judgment is required to ensure that the length and thickness of the undermined flaps are viable, as necrosis can compromise wound healing and result at worst in a failed reconstruction. If necessary, a Wise pattern is employed to tailor the skin flaps to an appropriately sized envelope. The reconstruction essentially involves the filling of a skin envelope with synthetic or autologous tissue, or both, and any NAC defect is replaced by a skin island from the flap.
The NAC has been shown to be free of cancer cells when there is no multifocal disease, the tumour is less than 2cm diameter, and there is greater than a 4 cm distance between the tumour and the NAC. This therefore applies particularly to risk reducing prophylactic mastectomy. The mastectomy may then be areola-sparing, or nipple and areola sparing. The nipple itself can be removed together with the mammary gland in one single specimen. The skin of a flap that reconstructs the breast mound can later be used for the nipple reconstruction together with re-approximation of the areola. Results of a retrospective study also show that a nipple sparing procedure may be used in relevant clinical circumstances.
Studies have now shown that “lumpectomy” or partial mastectomy (breast conserving surgery) with adjuvant radiotherapy is comparable to modified radical surgery not only in survival terms, but also in local recurrence rates. In early cases, therefore, therapeutic mammoplasty with radiotherapy, where after a local excision varying local reconstructive patterns are employed to reform the breast to an aesthetic shape, with or without contralateral surgery.
WHY CHOOSE BREAST MICROSURGERY?
The presence of breasts is a defining feature of adult mammalian gender. It must therefore be considered an essential element of human femininity, and the role it plays in female psychology cannot be understated. Breast cancer is a devastating disease for a number of reasons. Not only do sufferers have to face a scary and potentially life-threatening condition, but also the possibility of undergoing mutilating surgery to their breasts. The requirement for reconstruction of the female breast is almost exclusively consequent on breast surgery for breast cancer.
Due to the importance placed on a woman’s breasts, immediate reconstruction has been incredibly popular amongst patients who must undergo a mastectomy. Immediate reconstruction allows preservation of self- image, which is known to have a profound effect on the patient psyche and their overall wellbeing.
In general, breast reconstruction can be thought of as autologous (using body’s own tissues) or alloplastic (implant-based reconstruction). There are methods that utilise both autologous tissues as well as implants. Each patient – depending on their overall clinical picture, postoperative treatment regimen and personal preference – is considered as a unique case. Because of this, a tailored reconstruction plan is worked out to suit their specific needs.
WHAT IS A BREAST RECONSTRUCTION?
At Panthea Clinics, we aim to make this process less stressful by offering the most exceptional quality of care to each and every one of our patients. As experts in the field of breast microsurgery, our priority is always on you; providing you with the confidence and peace of mind knowing that you’re in the safe hands of experienced professionals.
Dr Farhadieh strongly believes in a multidisciplinary approach to breast cancer, which includes liaising with specific, specialty-based experts, such as general surgery, plastic surgery, general oncologists, radiation oncologists and nurses specialising in care for breast cancer patients. Because of this, he collaborates and cross-refers patients to general surgical colleagues. Women requiring breast cancer surgery as well as reconstruction will see Dr Farhadieh and one of his general surgery colleagues in order to devise a complete surgical plan.
WHAT ARE MY OPTIONS?
AUTOLOGOUS RECONSTRUCTION
Breast reconstruction has been achieved by replacing the removed breast tissue with the body’s own skin and fat for decades. The best areas to find tissue for breast reconstruction include the abdominal wall, inner thigh, buttocks and the back. During the surgical process, pedicled or free flap microsurgical techniques are generally used. Pedicled flaps are where the donor tissues are isolated on their blood supply and then moved to the breast without disconnecting this vascular supply. Free flap surgery, on the other hand, is where the tissues are disconnected from their blood supply and are reconnected to vessels near the breast using microsurgical techniques.
DEEP INFERIOR EPIGASTRIC PERFORATOR (DIEP) FLAP
Refinements of reconstructive surgery have meant that surgeons increasingly attempt to undertake major reconstructions with minimal complications at the donor site. Developed over 30 years ago, transverse rectus abdominis myocutaneous (TRAM) flaps – using muscle, fat and skin from the abdomen – were for many years the ‘gold standard’ method for breast reconstruction. TRAM flaps provided abundant tissues with good match for texture and consistency. The process of harvesting the TRAM flap included taking sections of the abdominal wall fascia (fibrous tissue layers) and underlying muscle along with abdominal wall fat and skin. However, it was found that for a significant number of patients the loss of the abdominal wall fascia led to a weakness in the wall and resulted in subsequent bulging.
More recently, the deep inferior epigastric perforator (DIEP) flap was developed to reduce the rates of these complications by allowing preservation of the abdominal wall fascia and muscle. It is a technically more demanding procedure but one that is increasing becoming standard treatment in major units around the world. Dr Farhadieh routinely provides DIEP reconstructions.
TRANSVERSE UPPER GRACILIS (TUG) MYOCUTANEOUS FLAP
When reconstructing smaller breasts, especially for bilateral reconstructions, one alternative method is to use the segment of the upper inner thigh for reconstruction. The blood supply to the gracilis muscle – an expendable inner thigh muscle – also supplies the overlying skin and subcutaneous fat. This allows the donor scar to be hidden in the inner thigh crease.
SUPERIOR/INFERIOR GLUTEAL ARTERY PERFORATOR (SGAP/IGAP) FLAPS
In a few cases, second-line autologous tissues need to be considered for breast construction. This can be due to a myriad of reasons, from patient preference to lack of other donor sites. The consistency of the gluteal (buttock) fat is not as soft as abdominal wall donor sites and therefore not as good a match for breast tissues. It is a technically more challenging surgery, but in some cases, it is the only suitable option.
ALLOPLASTIC RECONSTRUCTION
For many years, a two-stage reconstruction was standard alloplastic treatment for breast cancer. Tissue expansion with inflatable expanders would be performed in the first step and, after a period of waiting, the expanders were exchanged for silicone implants. With the advent of skin-sparing mastectomy, immediate implant-based reconstructions have become more common. When the nipple–areola area is retained, surgeons will attempt to preserve as normal a breast shape with the best-camouflaged scar possible. Where the nipple– areola complex has been removed, it can be reconstructed in day surgery approximately 3–6 months after reconstruction.
FAT INJECTION
In recent years, fat injection has become a common surgical option in the treatment of small contour deformities as well as radiation-induced chronic ulcers. Refinement of fat-harvesting techniques and isolation of fat cells has increased the survival rate for transferred fat cells. Interestingly, there is a growing body of evidence that some adult fat stem cells are capable of tissue rejuvenation by replenishing the local stem cell population and increasing capillary bed concentration. Although this holds the promise of tissue-engineered breast tissues from the patient’s own stem cells in the near future, the current indications for fat injections are predominantly for contour deficits. Mr Farhadieh has ongoing interest and involvement with stem cell-based tissue engineering research.